Abstract
Background:
Acute myeloid leukemia (AML) is a highly heterogenous condition. Current risk stratification based on cytogenetics and molecular genetic markers at point of diagnosis is used to predict treatment response and relapse risk. The conventional way of defining complete remission (CR) is based on morphological identification of ≤5% blasts seen in bone marrow. However, this does not provide adequate insight to the quality of response as there is still a high proportion of patients that relapse despite being in CR.
A significant proportion of AML patients have detectable MRD post induction. There is increasing evidence to support MRD as a significant prognostic factor for clinical outcome. Despite this, MRD status has yet to become an important factor in deciding on subsequent allogeneic stem cell transplant (allo-SCT). This study assessed the role MRD in predicting risk of relapse and survival rates and also looked into the role of allo-SCT in abrogating the adverse risk of MRD.
Methods:
All AML cases excluding acute promyelocytic leukemia who underwent curative chemotherapy from year 2001 until 2015 were retrospectively identified. Clinical data was gathered from computerized patient data system. Baseline patients and disease characteristic were correlated with post induction MRD status. MRD was assessed by flow cytometry analysis of bone marrow samples taken on day 26-30 days of post-induction. Samples from year 2001 to 2011 were analyzed using 4 color flow, and from 2011 onward, all samples were analyzed using 8 color flow. Leukemia-associated antigens were identified at baseline and followed up for MRD. Data collected were analyzed using SPSS Statistic Desktop V22.0.
Results:
235 patients underwent intensive chemotherapy. 61.7% achieved complete remission (CR) after induction chemotherapy. Among those who achieved CR after induction, 41.3% have detectable MRD. 42.8% eventually relapsed, after a median follow-up of 36.6 months. Median duration of CR was 49.5 months. The presenting WBC, LDH, time taken for neutrophil count or platelet count recovery after induction, cytogenetic risk group and FLT3-ITD and NPM1 molecular status did not correlate with MRD status.
Post induction MRD positive status was associated with higher relapse rate, 42.6% vs 22.4% for MRD positive and negative respectively, p=0.015, (OR = 1.9) (95% CI: 1.14-3.19).
In the multivariate analysis that include presenting WBC, LDH, BM blasts, risk group and post induction MRD status, risk group and MRD status remained an independent predictor for relapse. HR 1.95 (95% CI: 1.00-3.79), p=0.049 for positive MRD status, while adverse risk group gave a HR of 7.15 (95%CI: 2.01-25.49), p=0.002.
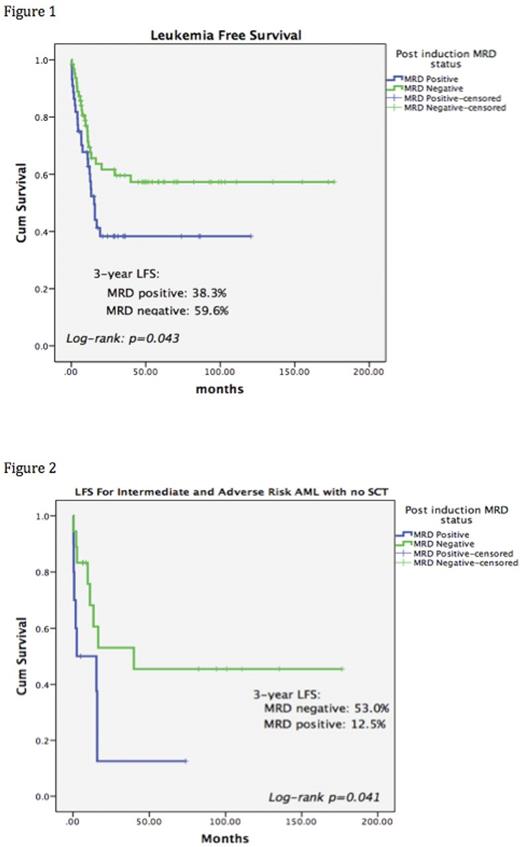
The 3-year Leukemia free survival (LFS) was 38.3% and 59.6% for MRD+ and MRD- group respectively (p=0.043) (figure 1), while the overall survival (OS) was 55.5% and 69.5% for MRD+ and MRD- group respectively (p=0.388).
55 patients underwent allo-SCT, 26 in MRD+ group and 29 in MRD- group. There was no statistical significance in terms of LFS among those who underwent allo-SCT according to MRD status (Median LFS were 13.1 months for MRD+, 29.2 months for MRD-, p=0.328). In the intermediate or adverse risk group who did not undergone allo-SCT, the median LFS in MRD+ group was only 2.5 months (95%CI: 0.0-21.2) compared to MRD- group, 39.9 months (p=0.041), (figure 2).
Conclusions:
Post induction MRD+ was associated with higher relapse rate and reduced LFS. Post induction MRD- status was associated with excellent LFS among AML with intermediate and adverse risk even without allo-SCT. Allo-SCT may be able to abrogate the adverse outcome of MRD+ AML.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal